The Success of Wireless Health Begins with Engineers
July 14, 2015

Healthcare is a universal need and its delivery a societal expectation. Today’s healthcare delivery, however, “tethers” the patient and the provider together episodically (i.e., requiring them to meet at a designated time and place).
Technology is an indispensable component of solutions for better care delivery, increased population coverage, and lower cost. Wireless health is a promising solution, enabling diagnosis, therapy and treatment regimen, and monitoring of health-related conditions by tracking biometric readings and relevant biomarkers while the patient goes about his or her daily life. Given its significant potential benefits to healthcare delivery systems and increasing patient demand for mobility, continued emergence of wireless health is a near certainty.
Wireless health finds its origin in care delivery in the developing world by leveraging the pervasiveness of wireless devices. Use cases have included education and awareness, remote data collection and monitoring, training and management of care personnel in the field, epidemic and disease tracking, and diagnostic and treatment support.
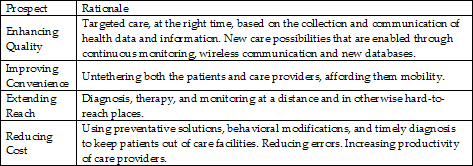
In the developed world wireless health solutions are motivated by a need to enhance quality, improve convenience, extend reach, and reduce the cost of care (see Table 1). Reducing cost is front and center, particularly in the US, where the quality of care is generally acceptable, convenience is a “nice-to-have,” and reach is generally not a pressing issue. The rising cost of care is, however, not sustainable and must be addressed -- making cost reduction a must have.
Annual healthcare expenditure in the US is projected at $3.3 trillion (i.e., $10,000 per person), well above other developed countries. Health spending annual growth rate has hovered around upper 3% since 2009; spending as a share of GDP has remained stable around 17.5%.
Healthcare expenditures are being escalated primarily by an aging population, longer life expectancy, and increased cases of chronic diseases such as hypertension, obesity, arthritis, asthma, diabetes, and chronic obstructive pulmonary disease (COPD). Chronic diseases alone account for 75% of US healthcare expenditures. And roughly 45% of the population has at least one chronic disease; about half of that number have two or more.
MORE FROM DESIGN NEWS: MEMS & Sensors Can Bring a New mHealth World
Advances in microsystems (e.g., sensors, actuators, electronics, batteries, displays, etc.) are enabling nonintrusive measurement of health and disease conditions, as well as delivery of therapy on demand. Connectivity and computing are ubiquitously available and at a low cost with high performance – and they will continue to get better with time. Social networks are a powerful tool for promoting peer comparisons and competitions in health and wellness, motivating behavioral change and providing support communities. Meanwhile, advances in genomics are ushering in a new era of personalized medicine.
The convergence of these technology trends will result in individualized, preventative medicine that is time and place independent. Figure 1 captures the key benefits of this convergence, recognizing the central role of wireless enablement; without wireless, the extent of each of the benefits is limited. Hence, the term “wireless health” should be emphasized over “mHealth,” “digital health,” or “connected health.” Nevertheless, these terms are often used interchangeably, even though they have been coined from different topical perspectives.

Wireless health is application-driven and technology-limited. Engineers are the key to developing and advancing technology solutions that expand use-case opportunities. Their effectiveness and efficiency, however, hinges on learning the basics of healthcare delivery systems and medical product development, as well as how to collaborate productively with clinicians.
In the context of the former, they need to learn the applicable regulatory policy and approval processes and reimbursement guidelines. In the context of the latter, they must learn basic medical terminology, as well as clinical roles, responsibilities, and workflows. While learning all of these may seem a huge undertaking, it is manageable by starting with introductory educational resources and building additional depth and breadth as needed.
MORE FROM DESIGN NEWS: 4 Reasons Why It's a Dynamic Time in Medical Device Design
Mehran Mehregany is the editor of a recent textbook titled “Wireless Health: Remaking of Medicine by Pervasive Technologies”. He is Goodrich Professor of Engineering Innovation at Case Western Reserve University, and dDirector of the Case School of Engineering San Diego programs.
About the Author(s)
You May Also Like





