Artificial Lung Is Microfluidics Marvel
August 4, 2011
In an important technical breakthrough, researchers at Case Western Reserve University have created a prototype artificial lung that functions with air -- just like human lungs.
Current artificial lungs require bulky compressed oxygen tanks. The CWRU invention creates the potential, several years down the road, for a portable or implantable artificial lung.
"Based on current device performance, we estimate that a unit that could be used in humans would be about six inches by six inches by four inches tall, or about the volume of the human lung. In addition, the device could be driven by the heart and would not require a mechanical pump," says Joseph Potkay, an electrical engineering and computer science professor at CWRU. The lung development was described in a paper in the research journal Lab on a Chip.
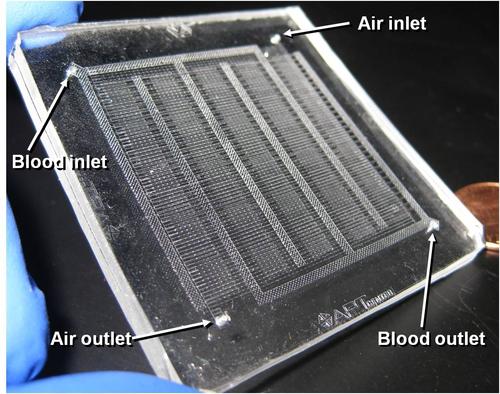
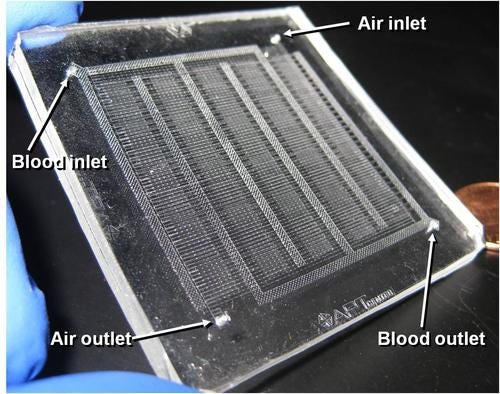
The prototype weighs about 20 grams (0.71 ounces). The scientists used breathable silicone rubber versions of blood vessels that branch down to a diameter less than one fourth that of human hair to build the prototype lung with a design that mimics the natural lung's tiny internal dimensions.
Researchers first built a mold with miniature features. Then they layered on a liquid silicone rubber that solidified into artificial capillaries and alveoli, and they separated the air and blood channels with a gas diffusion membrane. Potkay told Design News in an interview that his team built the mold with a pattern manufactured in a stereolithography machine using photo-sensitive polymers.
They were able to create a very large surface-area-to-volume ratio and shrink the distances for gas diffusion compared to the current state of the art by making the parts on the same scale as the natural lung. Tests using pig blood show that oxygen exchange efficiency is three to five times better than existing artificial lungs. This lets the researchers use plain air instead of pure oxygen as the ventilating gas.
Potkay, who specializes in micro- and nanotechnology, worked with Brian Cmolik, MD, an assistant clinical professor at the CWRU School of Medicine and a researcher at the Advanced Platform Technology (APT) Center and the cardiothoracic surgery department at the Louis Stokes Cleveland VA Medical Center. Michael Magnetta and Abigail Vinson, biomedical engineers and third-year students at the CWRU School of Medicine, joined the team and helped develop the prototype during the past two years.
Potkay's team is collaborating with researchers from Case Western Reserve's departments of biomedical engineering and chemical engineering to develop a coating to prevent clogging in the narrow artificial capillaries. They are also working on construction techniques to build a durable artificial lung large enough to test in rodent models of lung disease.
"We are starting to look at various ways to manufacture a larger-scale [closer to production] model," says Potkay. "Most of them are centered around additive manufacturing. We envision that silicone rubber will be utilized in future versions. We are, however, looking at various surface modifications of the silicone rubber in order to improve its biocompatibility and lifetime."
One issue going forward is the useful life of the artificial lung. Potkay told Design News that the first practical systems will have short lifetimes (less than a day) and will be used in acute applications, such as portable heart-lung machines. "As we make advancements in biocompatibility, we hope to have a device with a lifetime measured in months. Such a device would be suitable as a portable bridge to transplant for patients with severe lung disease."
Within a decade, the group expects to have human-scale artificial lungs in use in clinical trials. They envision that patients would tap into the devices while they allow their own diseased lungs to heal, or while they are waiting for a lung transplant -- a wait that lasts, on average, more than a year.
Potkay's work is being done in collaboration with the APT Center at the Louis Stokes Cleveland VA Medical Center, where he is an investigator. This work is currently funded by the US Department of Veterans Affairs.
Researchers at the Charles Stark Draper Laboratory in Cambridge, Mass., are also developing a silicone-based microfluidic artificial lung. They are targeting safer, more efficacious oxygenators by leveraging advanced microfabrication techniques capable of constructing biomimetic vascular networks with smooth blood flow paths that resemble the geometry of the human circulation.
"We have a laboratory prototype that we are testing with blood, and we are demonstrating oxygen transfer rates that, when the device is scaled up, will be clinically useful," Jeffrey T. Borenstein told Design News. He is Draper's principal investigator for projects involving the application of microsystems technology toward engineered tissue constructs for organ-assist devices.
The Draper project is funded by the National Heart, Lung, and Blood Institute.
About the Author(s)
You May Also Like



