Biomaterials
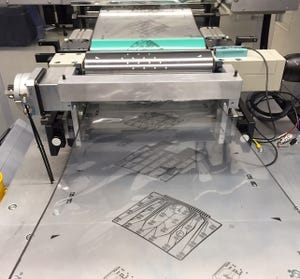
Bridge of Weir Leather introduces new methods of reducing the environmental impact of leather tanning.
Automotive Engineering
Bridge of Weir Leather Looks to Reduce Its Environmental ImpactBridge of Weir Leather Looks to Reduce Its Environmental Impact
Two new leather tanning processes slash the use of chrome, heavy metals, and aldehydes in the company’s signature leather automotive upholstery products.
Sign up for the Design News Daily newsletter.




















.jpg?width=300&auto=webp&quality=80&disable=upscale)


