May 19, 2011
Recoveryrates for American soldiers with head wounds are improving significantlybecause of new technology to quickly produce custom cranial implants that aremore resistant to infection.
More than 70cranial plates have been produced using the new process at WalterReed Army Medical Center (WRAMC) in Washington, D.C., with an averagesurgical time of 90 minutes from first incision to completion of suturing. Previously,the same types of surgeries took from two hours to more than six hours.
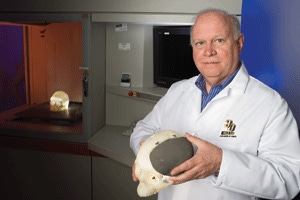
"The timesavings can be directly attributed to the improved implant design and attachedfixation," says Stephen L. Rouse, DDS, a government contractor working in the 3-D Medical Applications Lab at Walter Reed Army Medical Center. "Large implants were previously multi-piece constructs,and were slower to place and fixate."
High-Tech Implants_B |
At the heartof the process is advanced application of 3-D digital scanning and high-poweredadditive manufacturing equipment that can make highly accurate custom shapes inmedical-grade titanium alloys.
The originalsystems were based on lasers that created 3D shapes in processes calledstereolithography (SLA) and selective laser sintering (SLS). Both are ownedtoday by 3D Systems of Rock Hill, SC.
The rapidprototyping market gravitated to inexpensive 3D printers that can quickly makemodels from a wide range of materials, mostly plastic.
High-End Focus
Higher-endadditive manufacturing equipment is increasingly focusing on dental, medicaland aerospace applications, where engineers greatly value the ability to createprecise, complex, strong parts often not possible with injection moldingbecause of high costs or process limitations.
The work atWalter Reed improves life expectancy and quality of life for wounded soldiers.
One living,breathing example is Paul Statzer, who was a world champion weight lifter in2000. He was a veteran of the first Gulf War and decided to re-enlist. His unitwas sent to Iraq, and in 2005 he was investigating craters created by roadsidebombs. An improvised explosive device detonated near Sgt. Statzer, removingmuch of his skull, his eye and parts of his larynx.
He receivedemergency treatment in Iraq and Germany, and doctors told his family he mightnot survive.
W. LeeWarren, the surgeon who did the initial brain surgery on Sgt. Statzer at the332nd Air Force Theater Hospital in Balad, Iraq, says: "My memory of PaulStatzer was of a man so desperately injured that even while operating on him Igave him no chance for survival."
High-Tech Implants_A |
Followingemergency surgery and a transfer to Germany, Sgt. Statzer was taken to WalterReed where Rouse's lab performed a 3D scan of the cranial opening and made aplastic implant to replace the missing bone. Bone grafts and skin graftsreplaced the missing area around his left eye.
After monthsof rehabilitation, Sgt. Statzer learned to walk again and recovered most of hismemory.
Last year, Warrenhad a tearful reunion with his former patient in Pittsburgh near Sgt. Statzer'shome. He recalls the surgery in a recent book: "Called Out: A Brain SurgeonGoes to War."
SLA Master
The standardcranial implant is made from PMMA (polymethylmethacrylate). Astereolithography-produced master is embedded in a two-part flask. The masteris then removed and replaced by PMMA resin, which is then processed in alaboratory with pressure and heat.
"In largeimplant cases, the flask can weigh over 50 pounds, and is limited in contourcomplexity," says Rouse. Polishing, drilling for fixation and gas sterilizationusing ethylene oxide (EtO) is done prior to delivery to the operating room.
Onesignificant problem with that approach is that EtO sterilization equipment isnot available in many locations, and is being phased out or banned in manyhospitals because of environmental issues.
Analternative material used for transplants is PEEK (polyetheretherketone). Thegreat advantage of PEEK is its high-temperature tolerance (its glass transitionis 143C). PEEK can be autoclaved in any hospital operating room sterilizer,eliminating the requirement of gas or EtO sterilization.
PEEKimplants must be milled to exact shapes because of the expense of tooling.Rouse says that the cost of medical-grade PEEK blocks is very high.
According toindustry sources, medical grade PEEK costs close to $400 per pound compared toabout $44 per pound for industrial-grade PEEK. A leading medical-grade PEEKproducer declined to comment on the cost issue.
The biggestproblem, however, is that human tissue does not bond to plastic.
"Thisresults in loss of muscle attachment to the skull replaced by the implant, andthe formation of scar tissue which encapsulates the implant provides an areafor bacterial growth that cannot be reached by antibiotics," says Rouse. "Inpatients with history of antibiotic-resistant infections, this can result inthe loss of the implant if a recurrence of the infection appears."
The plasticcranial implants at Walter Reed needed to be removed about 12 percent of thetime to save the patient's lives.
New Approach
Rouse andthe surgical teams at Walter Reed brainstormed the implant problem.
Requirementsfrom surgeons included:
Standard available non-gassterilization methods;
Porosity in the implant to reduce trappedfluid pooling underneath;
Material compatibility with tissueingrowth to reduce the free space for infection;
Ability to conform to complexcontours and thickness changes, regardless of location; and
The implant needed to be visible onradiographs without causing radiographic artifacts and be safe to use MRI(magnetic resonance imaging).
"The onlymaterial available to us for this purpose is titanium alloy, with its provenbiocompatibility, strength and most importantly, its ability to promotefibrovascular ingrowth," says Rouse. "The only manufacturing method capable ofproducing such a complex geometric structure is additive-based."
Walter Reedofficials selected a new technology developed in Sweden by a company calledArcam using the electron beam melting technique (EBM).
Electron Beam
In the EBMprocess, fully dense metal parts are built up layer-by-layer as metal powder ismelted by a powerful electron beam. Each layer is melted to the exact geometrydefined by a 3D CAD model.
The buildtakes place in a vacuum at elevated temperatures, resulting in stress-relievedparts with material properties better than cast and comparable to wroughtmaterial, according to Magnus Rene, CEO of Arcam.
The vacuumsystem is designed to provide a base pressure of 1x10-4 or better throughoutthe entire build cycle. The EBM machine produces precise titanium mesh shapesthat allow bone ingrowth and prevent fluid pooling under the implant that canlead to infection.
Arcam's EBMtechnology is also used to make off-the-shelf orthopedic implants. Rene saysthat pores can be engineered to improve bone fixation. The goal is to improvebone ingrowth compared to current technologies of coating cobalt-chromeimplants with titanium beads or other materials.
The newimplant technology is working well at WRAMC.
Removalrates in the past three years have dropped to 4 percent. "None have had to beremoved following the healing process," says Rouse.
Other technologiessuch as Selective Laser Melting (SLM by MTT Technologies, Staffordshire, UK),and Direct Metal Laser Sintering (DMLS by EOS, Munich, Germany), were notavailable in the U.S. when Walter Reed began its testing.
The implantsare designed after segmenting CT scan data using Mimics software fromMaterialise that allows engineers to bridge 2D data to 3D. 3Matic, also fromMaterialise, and/or FreeForm Modeling Plus, from Sensable, are used for theactual implant design.
Sections canbe built in both mesh and solid, and the implant design includes the fixationplates. A skull model is created using a stereolithography machine and is sentwith the completed implant to the surgeon for approval.
Seven Day Limit
Speed is acritical factor.
"Our goal isto keep the entire process, from CT scan to delivery of the finished implant,to seven days," says Rouse. "In most cases, we are successful. Some of theissues, or problems that we have experienced include intermittent buildfailures, machine availability and shipping delivery delays."
One problemRouse has faced is lack of space for a program that is rapidly growing due toits huge success.
His fiveadditive manufacturing machines are scattered across the Walter Reed campuswhere space permits. That changes soon under the Base Realignment Program(BRAC), which is designed to make more efficient use of military assets.
Rouse'sgroup will soon move to a medical campus in Bethesda, MD, about six miles fromWRAMC, which is located near the outer border of Washington, D.C. The newcampus will be called the Walter Reed National Military Medical Center atBethesda.
Hisequipment and three-person staff will be in one location at the new medical center. Thatequipment includes an SLA 7000, SLA 500, Z Corp. 650, Z Corp. 450, and an ArcamA-1. On order is a Connex 500 from Objet Corp.
Theequipment serves a myriad of roles, ranging from pre- and post-surgical medicalmodels to custom cranial implants, subperiosteal dental implants, facial boneimplants and custom fixation devices.
Use of theadditive manufacturing machinery is not necessarily simple, unlike millingmachines, which can be left unattended.
They requiremonitoring to make sure there has been no warpage of the part. It's alsoimportant to ensure that the part is being produced to specification
Rouse saysthe Ti6Al4V powder must be monitored for oxygen content. The final part must betested to ensure that metallurgy is within specifications. Vigilant preventivemaintenance is required to make sure machines are available when needed. Unitslike the EBM machine are too expensive to have backups on hand.
"The bottomline for this entire process is the ability to build an implant that isdesigned for a specific patient's needs, that reduces the operating room timerequirement significantly, and provides better outcomes with more resistance toinfection," says Rouse.
About the Author(s)
You May Also Like







